What are Status and Status Reasons
The system applies a status and status reason to every claim. The status indicates the state or condition of the claim. The status reason provides additional information as to why the claim is in that state.
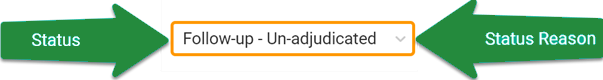
A user can view the claim's status/status reason on various pages throughout ZOLL Billing.
Here are some examples of status/status reason combinations:
- Closed - In collections
- Follow-up - Balance after refund
- Suspended - Verify COB
- Suspended - In state debt collections
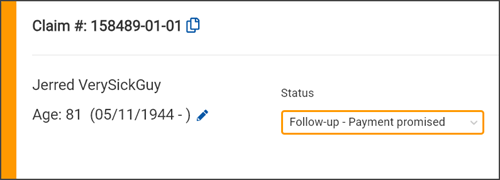
Changing a status and reason
On the Claim page, click the edit icon next to the status and status reason and then select one from the list.
You can change the status and reason on your claim whenever you want, with these exceptions:
-
Some status/status reasons are set by the system and cannot be changed (see the table below).
-
Once a claim is complete, you cannot move it back to Incomplete.
-
Once a claim has been billed, you cannot cancel it. The AR is on the books and if that is not right, then adjust off the balance.
-
You cannot close a claim with a balance.
-
You can’t move a claim to Credit Posted because that’s a pass through status and not a status your claim can sit in.
Overriding next payer/status
The payer and claim status can be overridden on the Transaction Details page (including 835 transactions). At the bottom of the page, under the "Next payer and status" heading, you will find two fields:
-
The first field will allow you to select the payer. When clicked, a list will display the payers from the COB, including the patient and the facility (if one exists on the COB). The payers will display in the order they exist on the COB (i.e. primary payer will display first, secondary payer second, etc.). If you move to a previous payer, the claim status field will default to the status associated with that payer unless the payer has not yet been billed. In that case the status will default to "Queued for submission" with the same override options as on the claim.
-
The second field will allow you to select the claim status. The color of the field's boarder will reflect the status you select.
There are several instances where you cannot change the payer or status:
-
The claim is in collections or state debt
-
The claim's balance is zero
-
Closed cannot be selected as a status
List of status & status reasons
The following table contains a list of all the statuses and their corresponding status reasons. A "yes" indicates that you can change this status and status reason combination to another combination. A "no" indicates the status and status reason combinations that are set by the system and therefore cannot be changed. You can search items within this table by entering the name in the search field. For example, if you want to see all the changeable statuses, enter "yes" in the search field. To see a specific status, enter the status name in search (i.e., Follow-up).
| Status name | Reason |
System sets =
User can set = |
|---|---|---|
| Appealed | ALJ |
 - yes - yes |
| Appealed | Appeal unresolved |
 - yes - yes |
| Appealed | Payer reprocessing |
 - yes - yes |
| Appealed | Phone appeal |
 - yes - yes |
| Appealed | Reconsideration |
 - yes - yes |
| Appealed | Redetermination |
 - yes - yes |
| Appealed | Written appeal |
 - yes - yes |
| Canceled | Duplicate claim |
 - yes - yes |
| Canceled | Mutual aid service |
 - yes - yes |
| Canceled | Patient deceased |
 - yes - yes |
| Canceled | Patient is a city employee |
 - yes - yes |
| Canceled | Patient is a prisoner |
 - yes - yes |
| Canceled | Patient not found |
 - yes - yes |
| Canceled | Patient refusal |
 - yes - yes |
| Canceled | Unbillable |
 - yes - yes |
| Closed | Balance resolved |
 - yes - yes |
| Closed | In collections |
 - no - no |
| Closed | Payer paid the patient |
 - yes - yes |
| Closed | Refund |
 - no - no |
| Closed | Review non-collections activity |
 - no - no |
| Closed | Write-off (full) |
 - no - no |
| Closed | Write-off (partial) |
 - no - no |
| Credit posted | Collections fee |
 - no - no |
| Credit posted | Payment |
 - yes - yes |
| Credit posted | Payment reversal |
 - no - no |
| Credit posted | Refund |
 - no - no |
| Credit posted | Refund adjustment |
 - no - no |
| Credit posted | Revenue adjustment reversal |
 - no - no |
| Credit posted | Take back |
 - no - no |
| Credit posted | Write-off |
 - no - no |
| Credit posted | Write-off reversal |
 - no - no |
| Denied | Appeal needed |
 - no - no |
| Denied | Appeal request rejected |
 - no - no |
| Denied | Denial unresolved |
 - yes - yes |
| Denied | Denial upheld |
 - no - no |
| Denied | Full denial |
 - no - no |
| Denied | Partial denial |
 - no - no |
| Denied | Payer reprocessing |
 - yes - yes |
| Follow-up | Account review |
 - no - no |
| Follow-up | Balance after adjustment |
 - no - no |
| Follow-up | Balance after refund |
 - no - no |
| Follow-up | Balance after refund reversal |
 - no - no |
| Follow-up | Balance after take back reversal |
 - no - no |
| Follow-up | Balance forwarded |
 - no - no |
| Follow-up | Charges corrected after submission |
 - no - no |
| Follow-up | Clinical documentation requested |
 - yes - yes |
| Follow-up | Credit balance |
 - no - no |
| Follow-up | Credit from ineligible payer |
 - no - no |
| Follow-up | Deductible variance |
 - no - no |
| Follow-up | In medical review |
 - yes - yes |
| Follow-up | LOA overpayment |
 - no - no |
| Follow-up | LOA underpayment |
 - no - no |
| Follow-up | No response from payer |
 - no - no |
| Follow-up | Overpayment |
 - yes - yes |
| Follow-up | Patient involvement needed |
 - yes - yes |
| Follow-up | Payer paid the patient |
 - yes - yes |
| Follow-up | Payer reprocessing |
 - yes - yes |
| Follow-up | Payment activity against obsolete charge |
 - no - no |
| Follow-up | Payment move requested |
 - yes - yes |
| Follow-up | Payment moved |
 - no - no |
| Follow-up | Payment plan not met |
 - yes - yes |
| Follow-up | Payment promised |
 - yes - yes |
| Follow-up | Payment reversal |
 - no - no |
| Follow-up | Payment review needed |
 - no - no |
| Follow-up | Reconsideration |
 - yes - yes |
| Follow-up | Refund requested |
 - yes - yes |
| Follow-up | Review non-collections activity |
 - no - no |
| Follow-up | Review requested |
 - no - no |
| Follow-up | Take back |
 - no - no |
| Follow-up | Take back (pending) |
 - yes - yes |
| Follow-up | Un-adjudicated |
 - no - no |
| Follow-up | Underpayment |
 - yes - yes |
| Follow-up | Verify COB |
 - yes - yes |
| Incomplete | Charge needed |
 - yes - yes |
| Incomplete | Coding needed |
 - yes - yes |
| Incomplete | Facility needed |
 - yes - yes |
| Incomplete | New claim |
 - yes - yes |
| Incomplete | Payer needed |
 - yes - yes |
| Incomplete |
Verify patient account *This status only displays for imported claims that need patient verification. After the information is verified, the claim is created and the status changes to Incomplete - New claim. |
 - no - no |
| Queued for submission | Clearinghouse |
 - yes - yes |
| Queued for submission | Facility invoice |
 - yes - yes |
| Queued for submission | Manual submission |
 - yes - yes |
| Queued for submission | New claim |
 - yes - yes |
| Queued for submission | Patient statement |
 - yes - yes |
| Queued for submission | Resubmit statement |
 - no - no |
| Submitted | Auto crossover |
 - yes - yes |
| Submitted | Clearinghouse |
 - no - no |
| Submitted | Facility invoice |
 - yes - yes |
| Submitted | Final statement sent |
 - no - no |
| Submitted | Manual submission |
 - no - no |
| Submitted | Manual upload |
 - yes - yes |
| Submitted | New claim |
 - no - no |
| Submitted | Patient statement |
 - yes - yes |
| Suspended | Account locked |
 - no - no |
| Suspended | Account review |
 - no - no |
| Suspended | Adjustment needed |
 - yes - yes |
| Suspended | Adjustment requested |
 - yes - yes |
| Suspended | Auth appealed |
 - yes - yes |
| Suspended | Auth denied |
 - yes - yes |
| Suspended | Auth primary needed |
 - yes - yes |
| Suspended | Auth requested |
 - yes - yes |
| Suspended | Auth secondary needed |
 - yes - yes |
| Suspended | Charge needed |
 - yes - yes |
| Suspended | Claim against estate filed |
 - yes - yes |
| Suspended | Claim against estate needed |
 - yes - yes |
| Suspended | Clearinghouse |
 - no - no |
| Suspended | Clinical documentation needed |
 - yes - yes |
| Suspended | Clinical documentation received |
 - yes - yes |
| Suspended | Clinical documentation requested |
 - yes - yes |
| Suspended | Coding needed |
 - yes - yes |
| Suspended | Collection letter sent |
 - yes - yes |
| Suspended | Credit balance |
 - no - no |
| Suspended | Designation changed |
 - no - no |
| Suspended | Diagnosis review needed |
 - yes - yes |
| Suspended | Doc packet needed |
 - yes - yes |
| Suspended | Eligibility check needed |
 - no - no |
| Suspended | Eligibility checks not available for payer |
 - no - no |
| Suspended | Face sheet requested |
 - yes - yes |
| Suspended | Facility needed |
 - yes - yes |
| Suspended | Failed validation |
 - no - no |
| Suspended | Final statement sent |
 - no - no |
| Suspended | Hold for deductible |
 - yes - yes |
| Suspended | Hold for retroactive Medicaid |
 - yes - yes |
| Suspended | In state debt collections |
 - no - no |
| Suspended | In active coverage |
 - no - no |
| Suspended | Insurance needed |
 - yes - yes |
| Suspended | LOA needed |
 - yes - yes |
| Suspended | LOA pending |
 - yes - yes |
| Suspended | Medicaid pending |
 - yes - yes |
| Suspended | Medical necessity appeals |
 - yes - yes |
| Suspended | Medical records request |
 - yes - yes |
| Suspended | Network approval needed |
 - yes - yes |
| Suspended | Next payer needed |
 - no - no |
| Suspended | Past timely filing |
 - yes - yes |
| Suspended | Patient address needed |
 - no - no |
| Suspended | Patient agreement needed |
 - yes - yes |
| Suspended | Patient bankruptcy |
 - yes - yes |
| Suspended | Patient covered by Medicaid |
 - yes - yes |
| Suspended | Patient deceased |
 - yes - yes |
| Suspended | Patient grievance |
 - yes - yes |
| Suspended | Patient is a member |
 - yes - yes |
| Suspended | Patient is homeless |
 - no - no |
| Suspended | Payer address needed |
 - no - no |
| Suspended | Payer needed |
 - yes - yes |
| Suspended | Payment plan disabled |
 - no - no |
| Suspended | PCR addendum needed |
 - yes - yes |
| Suspended | PCS needed |
 - yes - yes |
| Suspended | PCS requested |
 - yes - yes |
| Suspended | Pending legal |
 - yes - yes |
| Suspended | Pre-determination needed |
 - yes - yes |
| Suspended | Referral needed |
 - yes - yes |
| Suspended | Refund needed |
 - yes - yes |
| Suspended | Review new claim |
 - yes - yes |
| Suspended | Signature needed |
 - yes - yes |
| Suspended | Verify claim balance |
 - no - no |
| Suspended | Verify COB |
 - yes - yes |
| Suspended | Verify coverage |
 - no - no |
| Suspended | Write-off pending |
 - yes - yes |


